-
Published4 hours ago
The NHS continued to give patients infected blood after virus screening had been introduced in the UK.
Screening, including for hepatitis C, began in September 1991 but there was no process to stop old, contaminated blood being used.
BBC News has learned untested and potentially contaminated blood could have been stored for up to 10 years.
We have identified patients infected after 1 September 1991, who are currently unable to claim compensation.
Schemes for victims to claim financial compensation are only open to those treated with infected blood prior to the introduction of routine virus screening.
Lawyers have told BBC News the rules about eligibility should be changed.
‘Fighting for every crumb’
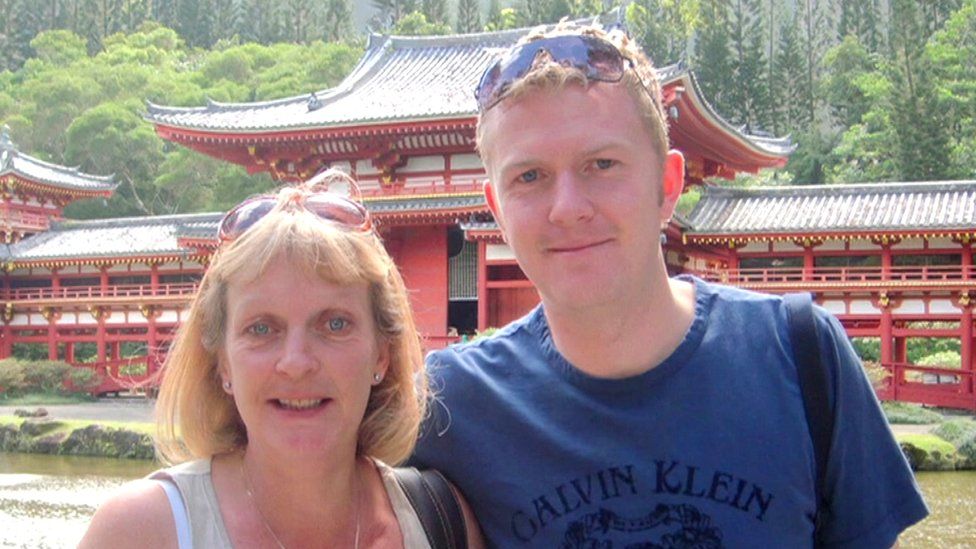
Caz Challis was diagnosed with cancer in 1992 and received several blood transfusions over the next 12 months. In 1993, she was diagnosed with hepatitis C before undergoing a stem cell transplant.
The NHS trust where she was treated has confirmed the virus came from blood she received during her cancer treatment.
She is one of many victims who are not eligible for compensation. She says she has been left “fighting for every crumb” and feeling “that you don’t count”.
Beatrice Morgan, a solicitor at law firm Leigh Day, represents more than 300 infected blood victims. She is calling for compensation schemes to be extended to those who received infected blood beyond the date routine screening was introduced.
“Although there was a national rollout of testing of new donations from 1 September 1991, blood that was already in the system wasn’t tested,” Ms Morgan says. “We have evidence to show that there was untested blood that slipped through the net.”

The infected blood scandal is one of the biggest treatment disasters in NHS history – 3,000 people who were infected with HIV and hepatitis C after being given contaminated blood and blood products have died.
Many victims were haemophiliacs and were given infected blood products as part of their treatment. But thousands more were given transfusions using contaminated blood after accidents, emergencies or childbirth.
After years of campaigning by victims, the Infected Blood Inquiry was announced in 2017. Led by former judge Sir Brian Langstaff, it heard evidence between 2019 and 2023.

During hearings at the inquiry, several doctors confirmed untested blood remained within the NHS supply after virus screening began.
“There was quite a lot of uncertainty about what we were doing,” Dr Frank Boulton, who was working in the west of England at the time, said. “I did feel a little bit nervous about the chance of HCV [hepatitis C] emerging amongst some of our recipients.”
Giving evidence, blood expert Professor Marcela Contreras told the inquiry that in some parts of the country there was blood in the system which had not been tested for viruses, including HIV, until as late as October 1995. Some rare blood groups “could be frozen for 10 years”, she added.
Concerns about remaining untested blood product stocks in the system being administered to patients had been raised by doctors before screening was introduced.
In February 1991, Dr John Cash, from the Scottish National Blood Transfusion Service, wrote a letter to Dr Harold Gunson, who at the time was director of the National Blood Transfusion Services.
He asked when a decision would be made about whether existing blood stocks would be tested, noting: “The task is doable but formidable.”
No national policy was ever announced and testing was piecemeal, if it happened at all.
During the Infected Blood Inquiry, Sir Brian Langstaff noted some old blood donations were not tested, saying: “If it’s right, it may have repercussions for the accuracy of the start date [of the compensation schemes].”
The inquiry into the wider infected blood scandal will conclude on 20 May.

BBC Wales Investigates: Blood Money
How did 3,000 people lose their lives to deadly diseases in blood? Wyre Davies exposes the role of drugs companies, politicians and doctors.
Watch now on BBC iPlayer (UK only)

-
-
Published14 April

-
-
-
Published14 hours ago
-
-
-
Published18 April
-
