-
Published2 days ago
This video can not be played
To play this video you need to enable JavaScript in your browser.
When 10-month-old Colin Smith contracted HIV after receiving contaminated blood, his parents’ house was daubed with “Aids dead”.
His father was also forced to leave his job.
Now 34 years on from his death from Aids at the age of seven, his family are facing another injustice.
A BBC investigation has found Prof Arthur Bloom, the doctor who gave Colin infected imported blood product Factor VIII, broke his own rules to do so.
Just three months earlier, Prof Bloom’s own department had written internal NHS guidelines discouraging the use of imported blood treatments on children because of the risk of infection.
“This wasn’t an accident,” said Colin’s father, also called Colin. “It could have been avoided.”
His son, who was being treated for haemophilia – a rare condition that affects the blood’s ability to clot – was one of more than 3,000 people to die in the UK after being given infected blood products.
Parents Janet and Colin, from Newport, have fought for more than 40 years for answers and hope the infected blood inquiry, which is due to report its findings next month, will provide a measure of closure.
In January 1982, more than a year before Prof Bloom first treated Colin, he co-wrote a letter to all haemophilia centres calling on them to give patients new heat-treated products aimed at destroying viruses.
He said they should be administered to previously untreated patients (PUPs) not yet exposed to high-risk American products, much of which were bought from donors such as prison inmates and drug-users.
The letter explained the previous trials on chimpanzees were no longer suitable and they needed humans to test on.
BBC Wales Investigates has discovered internal NHS guidelines from May 1983 for the department Prof Bloom was in charge of that discouraged the use of imported blood treatments on children because of the risks of infection.
But just three months later, Prof Bloom ignored his own rules when treating Colin.
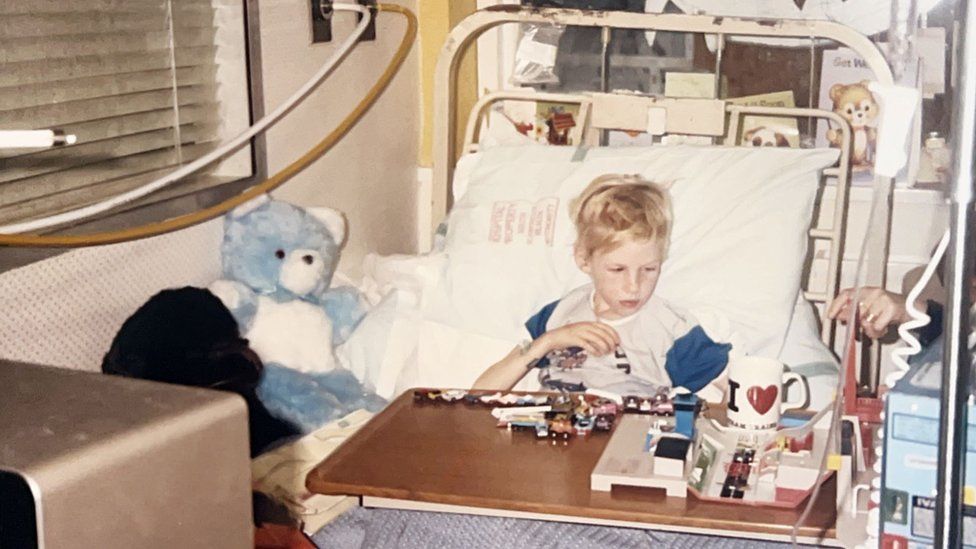
Colin was infected with HIV and hepatitis C in August 1983 after being given blood products imported from the US. He died in 1990.
Prof Bloom died in 1992.
Colin and Janet believed their son was being experimented on with new heat-treated Factor VIII which, it was hoped, would kill viruses like HIV and hepatitis.
“He just happened to be diagnosed with haemophilia at the same time these trials were starting up – the next thing you know he’s got HIV,” said Janet.
Colin senior said: “They were playing Russian roulette with people’s lives, and they miscalculated and killed thousands.”
Janet said the family were told about Colin’s HIV diagnosis in a busy hospital corridor.
“Colin was lying in bed, not well at all, and Prof Bloom stops in the corridor and just said ‘he’s HIV’,” she said.
“We were never taken to a room, we were told in the middle of the corridor, parents running after their kids, little kiddies running past us, and I can remember getting really upset but I don’t know why because it was never explained that it was a death sentence.”
Janet and Colin only found about their son’s hepatitis C diagnosis several years later.

In the 1980s fear, stigma and discrimination towards people with HIV and Aids was commonplace.
The UK government’s 1987 Aids awareness advert – with actor John Hurt’s haunting delivery of “it’s a deadly disease with no known cure” to a backdrop of falling tombstones – added to the public’s perception of HIV.
As their son’s health deteriorated, Colin’s parents were ostracised by the local community in Newport.
“We were known as the Aids family,” said Janet.
“We’d have phone calls 12, one o’clock in the morning. ‘How can you let him sleep with his brothers? He should be locked up, he should be put on an island’… he was three.”
“It got out of hand,” said Colin senior. “One day we got up and ‘Aids dead’ was written right across the side of the house [in] black paint.”
This video can not be played
To play this video you need to enable JavaScript in your browser.
Colin senior said he became “unemployable” because of the stigma surrounding the virus.
“I got a new job delivering milk, believe it or not I had a phone call the morning after I was due to start and they said ‘sorry, somebody’s told us there’s HIV in the family, we can’t start you’.”
BBC Wales Investigates also uncovered documents that revealed doctors were willing to accept a riskier product in order to keep costs down.
Papers show Immuno – the now dissolved drug company that made the Factor VIII given to Colin – thought the UK market would accept a riskier product made from imported US blood over safer European blood because it was cheaper to import.
“You get to a stage when you read things like that, to us it was murder,” Janet said. “They were saving pennies, basically you treat them on the cheap.
“They weren’t worried about people’s health as far as I’m concerned.”
Why did the infected blood scandal happen?
The scandal has been called the biggest treatment disaster in NHS history and decades on victims are still campaigning for compensation.
In the 1970s, the UK was struggling to meet the demand for blood-clotting treatments, so imported supplies from the US.
But much of the blood was bought from high-risk donors such as prison inmates and drug-users.
Factor VIII was made by pooling plasma from blood from tens of thousands of donors. But if just one person was carrying a virus, the entire batch could be contaminated.
In 1975, several years before the first known cases of HIV, a documentary exposed the risks of imported blood products from the US being infected with viruses and the government pledged to become self-sufficient in the UK.
Prof Edward Tuddenham, who was treating haemophiliacs at this time, said it was understood the products were risky.
“[Health minister] David Owen had announced the government policy for self-sufficiency which was the World Health Organisation recommendation, but that quietly got dropped,” he said.
“It was cheaper to import from America. It was clear that there was hepatitis being transmitted and that was apparent by the late seventies.”
He added: “At the end of the day, the bottom line is what matters. And they [drugs companies] had a product that they were making a lot of money from.
“So, there was a natural tendency to wish to carry on pushing that even as the risk became more and more obvious.”

By 1983, a new virus known as HIV was spreading across the world.
Despite early warnings and growing evidence, government officials and ministers in the UK repeatedly told the public there was ‘no conclusive proof’ that it could be transmitted through imported blood products.
The blood services began routinely screening donations for HIV in 1985 and screening for hepatitis C in 1991.
The UK-wide infected blood inquiry was announced in 2017 after years of campaigning by victims. It was led by former judge Sir Brian Langstaff, and took evidence between 2019 and 2023.
The inquiry will publish its report on 20 May.
-
-
Published2 April

-
-
-
Published22 June 2023

-
-
-
Published8 February

-
