-
Published19 hours ago
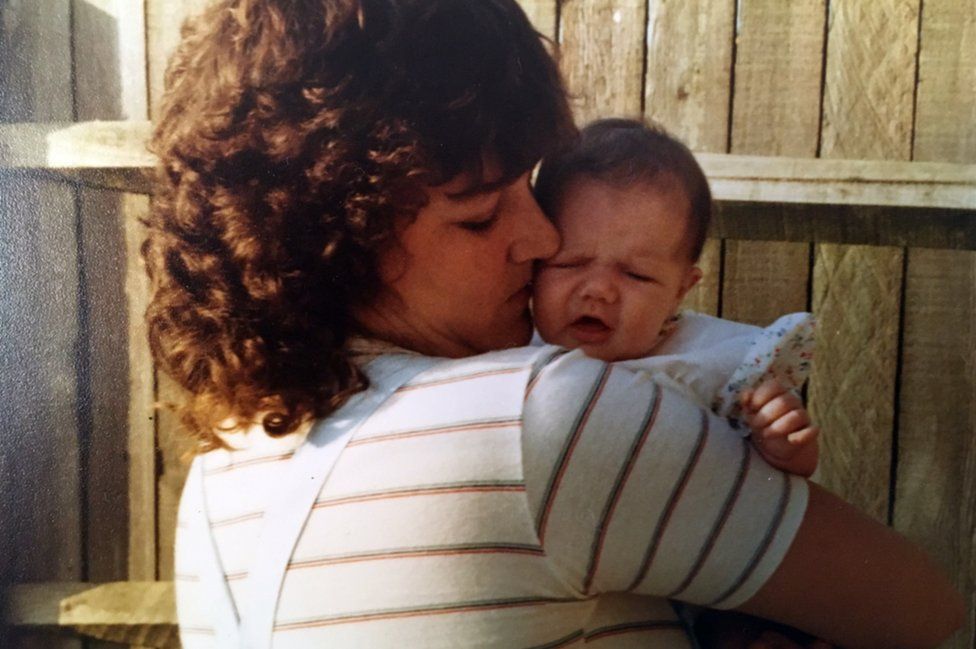
Thousands of people in the UK were infected with HIV and hepatitis C after being given contaminated blood products during the 1970s and 1980s.
A public inquiry into what has been called the biggest treatment disaster in NHS history will publish its findings in May, but victims are still campaigning for compensation.
Who was affected by the infected blood scandal and how many patients were involved?
Two main groups of NHS patients were caught up in the scandal.
Firstly, haemophiliacs – and those with similar disorders – who have a rare genetic condition which means their blood does not clot properly.
People with haemophilia A have a shortage of a clotting agent known as Factor VIII. People with haemophilia B don’t have enough Factor IX.
In the 1970s, a new treatment was developed to replace the missing clotting agents, made from donated human blood plasma.
But whole batches of the replacement Factor VIII and IX products were contaminated with deadly viruses.
The infected blood inquiry estimates that 1,250 people with bleeding disorders in the UK developed both HIV and hepatitis C as a result, including 380 children.
Around two-thirds later died of Aids-related illnesses. Some of those infected unintentionally gave HIV to their partners.
Another 2,400 to 5,000 people developed hepatitis C on its own, which can cause cirrhosis and liver cancer.
This video can not be played
To play this video you need to enable JavaScript in your browser.
The second group of patients were given a contaminated blood transfusion after childbirth, surgery or other medical treatment between 1970 and 1991.
Estimating the size of this group is difficult, but the inquiry thinks up to 100 may have been infected with HIV, and between 21,000 and 39,000 with hepatitis C.
Why did the infected blood scandal happen?
In the 1970s, the UK was struggling to meet the demand for blood-clotting treatments, so imported supplies from the US.
But much of the blood was bought from high-risk donors such as prison inmates and drug-users.
Factor VIII was made by pooling plasma from tens of thousands of donors.
If just one was carrying a virus, the entire batch could be contaminated.
UK blood donations were not routinely screened for hepatitis C until 1991, 18 months after the virus was first identified in a laboratory.
What did the authorities know about infected blood?
By the mid-1970s, there were repeated warnings that imported US Factor VIII carried a greater risk of viral infection.
But attempts to make the UK more self-sufficient in blood products in the following years failed, so the NHS continued to use foreign supplies.
Campaigners say haemophiliacs could have been offered an alternative treatment called Cryoprecipitate. This was less effective and harder to administer, but was made from the blood plasma of a single donor, lowering the infection risk.
As late as November 1983, the government insisted there was no “conclusive proof” that HIV could be transmitted in blood, a line robustly defended by former health minister Ken Clarke when he appeared before the inquiry.
By April 1985, all Factor VIII products were heat-treated to kill the HIV virus.
This video can not be played
To play this video you need to enable JavaScript in your browser.
When was the infected blood inquiry set up and when will it report?
The UK-wide infected blood inquiry was announced in 2017 after years of campaigning by victims.
It was led by former judge Sir Brian Langstaff, and took evidence between 2019 and 2023.
The inquiry will publish its report on 20 May.
It had been expected in autumn 2023, but Sir Brian said more time was needed to prepare “a report of this gravity”.
Who gave evidence to the inquiry?
One of the first to take the stand was Derek Martindale, who has haemophilia. He was diagnosed with HIV and given a year to live in 1985, aged 23. He survived but his brother – who was also infected with HIV – did not.
The inquiry also heard harrowing testimony from former pupils at Treloar’s, a specialist boarding school in Hampshire, where dozens of young haemophiliacs were infected with HIV.
Specialist haemophilia doctors working at the time also gave evidence.
As well as Lord Clarke, the inquiry heard from former and current ministers in all four UK nations, including Prime Minister Rishi Sunak and Chancellor Jeremy Hunt.
Will victims of the infected blood scandal get compensation?
Those infected have received annual financial support from the government, but a final compensation deal has not been agreed.
In late 2022, following advice from the inquiry, the government made interim payments of £100,000 each to around 4,000 surviving victims and some bereaved partners.
In April 2023, Sir Brian said interim compensation should also be offered to the children and parents of those infected.
He also recommended a final compensation scheme be set up, with the total cost likely to run into billions.
The government said it would be “inappropriate” to consider final compensation payments ahead of the inquiry’s full report.
What happened in other countries which were affected by inflected blood?
Many other countries were affected by the same scandal, although some – including Finland – were self-sufficient in Factor VIII, which minimised HIV infections.
In the US, companies that supplied infected products have paid out millions of dollars in out-of-court settlements.
Politicians and drug companies have been convicted of negligence in other countries, including France and Japan.
In his evidence to the inquiry, former health secretary Andy Burnham suggested there may be grounds for charges of corporate manslaughter in the UK.
