-
Published56 minutes ago
Changing how children are measured for obesity to a new system could be more accurate, a study has concluded.
It revealed the traditional method of using Body Mass Index (BMI) is not as useful in measuring fat as waist-to-height ratio (WHtR).
Over a 15-year follow-up, 7,237 nine-year-old children were studied.
The findings could change guidelines that recommend BMI as a measure. Researchers said it was critical to accurately detects obesity in children.
The Bristol project, the Avon Longitudinal Study of Parents and Children (ALSPAC), was published in the journal Paediatric Research.
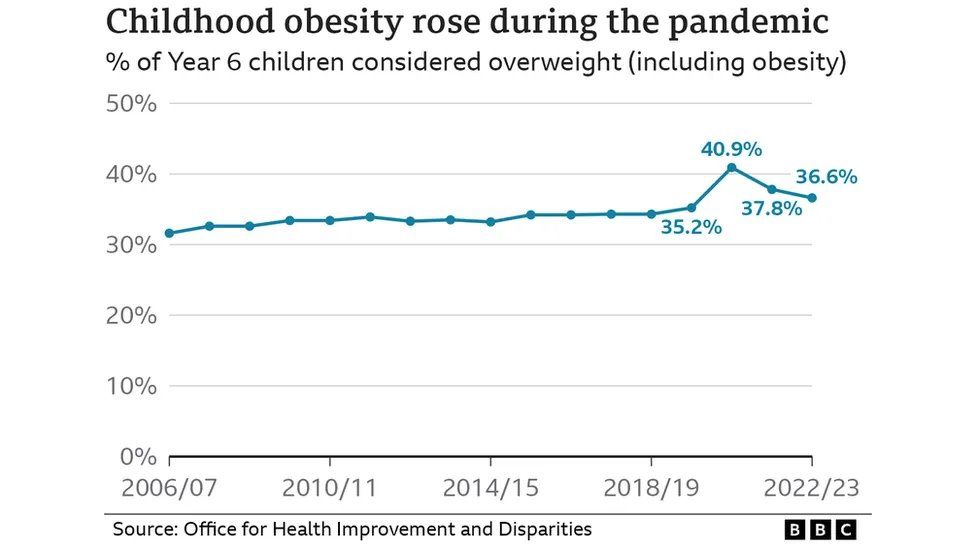
Obesity rates rose sharply among 10 and 11 year olds in England during the Covid pandemic and have not returned to pre-pandemic levels.
Professor Julian Hamilton-Shield, a consultant paediatrician at the Bristol Royal Hospital for Children, said his weight management clinic is now seeing a lot more patients with obesity-related diseases.

He added: “We are seeing more severe levels of obesity and and we are seeing more severe complications.
“So in order to be able to pick that up we need to have good measures that tell us more about people’s health.”
Between 2019-2020 and 2020-2021, the proportion of overweight and obese Year 6 primary school children, aged between 10 and 11, went from 35.2% to 40.9%, with people from deprived areas disproportionately affected.
Researchers used BMI data from the government’s National Child Measurement Programme, which weighs and measures about a million Year 6 pupils annually in England.
Body Mass Index (BMI) has long been the go-to tool for determining a healthy weight. It’s a simple and quick way to check and is a measure of body fat based on height and weight.
However, many health practitioners now use the waist-to-height ratio method in addition. This is because BMI doesn’t take into account a person’s body frame or muscle mass.
However, this scale has recently been called outdated by some groups as it would place a rugby player, for example, in the obese category.

Researchers from the University of Bristol, the University of Exeter, and the University of Eastern Finland have found one option that could replace BMI, and said that it can more accurately measure excess fat mass in children and adolescents.
Lead author, Professor Andrew Agbaje said that the waist circumference-to-height ratio is an inexpensive way to determine excess fat mass and distinguish muscle mass from fat mass.
Professor Agbaje added: “With just a measuring tape we can dictate eight out of ten children who are truly fat and the second thing is we can also detect 93 out of 100 who are not fat at all, who are just muscular.
“So we can detect 93 of those people who are not truly fat whom BMI would have judged had been overweight and obese as not having a problem with fat at all.”
He said that BMI varies with age and sex, but waist-to-height ratio stays the same irrespective of age and sex.

Follow BBC Bristol on Facebook, X and Instagram. Send your story ideas to us on email or via WhatsApp on 0800 313 4630.
-
-
Published24 January

-
