There are two opposite paths to achievement in science. The first is straightforward: Identify a problem and set about solving it. The second is rather unscientific-sounding and perhaps more faith-based: Study in obscurity and hope serendipity strikes.
In 1980, a young gastroenterologist named Jean-Pierre Raufman wound up taking the latter road through the digestive-diseases branch of the National Institutes of Health. His goal there was to gain research experience. While doing so, he chanced to meet the lead chemist of another laboratory, John Pisano, who had a passion for seeking out new and interesting examples of a specific kind of hormone, called a peptide, in animal venoms. Pisano regularly appealed to local insect and reptile enthusiasts in the classified pages of The Washington Post; in response, they would show up at his office door carrying plastic bags wriggling with possibility.
Pisano offered some venom samples to Raufman for his meandering analyses. Over the following month, Raufman experimented with them to see if they stimulated pancreatic cells harvested from guinea pigs. The venom with the biggest effect by far came from a desert reptile that Raufman had never heard of: the Gila monster.
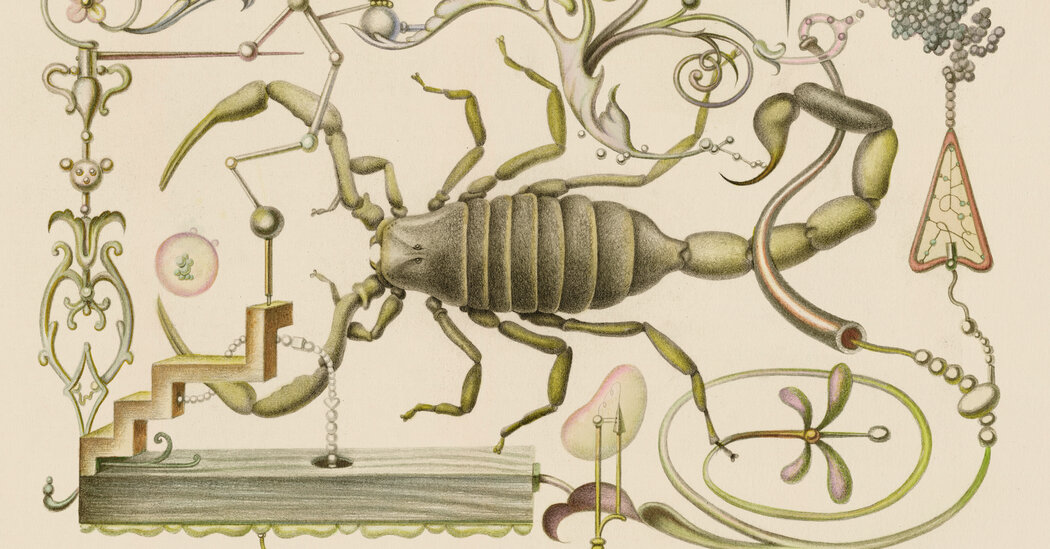
Gila monsters — sluggish, thick-tailed ground dwellers — are native to southern Arizona and northern Mexico. They have blunt noses and bumpy black skin with tan, pink or orange squiggles. They spend 95 percent of their lives underground. Like their cousins to the south, Mexican beaded lizards, they are one of the very few lizard species that produces venom, which they excrete from mouth glands into grooves in their serrated teeth. The strength of their jaws is typically enough to subdue their prey (chicks, frogs, worms and the like). But if threatened and unable to escape or hide, they may bite a predator. Whenever they clamp down, piercing the skin, venom enters the victim’s bloodstream. This causes intense pain and can initiate a cascade of other symptoms that, in people, includes vomiting, dizziness, rapid heart rate, low blood pressure and, in rare circumstances, death.
Raufman experimented with the Gila-monster venom for a while, then moved on to other projects. Years passed. He took a faculty position at what was then the State University of New York Health Science Center in Brooklyn and set up his own lab. Soon he found himself collaborating with a group at the Veterans Affairs Medical Center in the Bronx. One of the scientists there, an endocrinologist named John Eng, was impressed by Raufman’s work with the Gila monster. He was especially intrigued by its glacial metabolism — the lizard can survive on fewer than a handful of meals per year. Eng and Raufman paired up, screened the venom again and found molecules Raufman had not observed before. They called these molecules exendin-3 and -4.
Eng recognized the exendins as a potential diabetes therapy. He had patients with the condition who needed to calibrate their insulin injections carefully to avoid both hyper- and hypoglycemia. Exendin-4, on the other hand, resembled a human hormone called GLP-1, which works as a natural insulin manager in people without diabetes. When we eat, the small intestine releases GLP-1, prompting the pancreas to produce more insulin only when blood-sugar levels get too high. The molecule also slows digestion and makes us feel full. Scientists suspected that injections of GLP-1 would be a much easier and safer diabetes treatment than insulin, except for one crucial problem: The hormone lasts only a few minutes in the bloodstream before it breaks down. But the Gila monster analogue, Eng and Raufman were surprised to note, lasts for hours.