As videos describing the procedure as agonizing spread on social media, new guidelines advise physicians to consider various anesthetics.
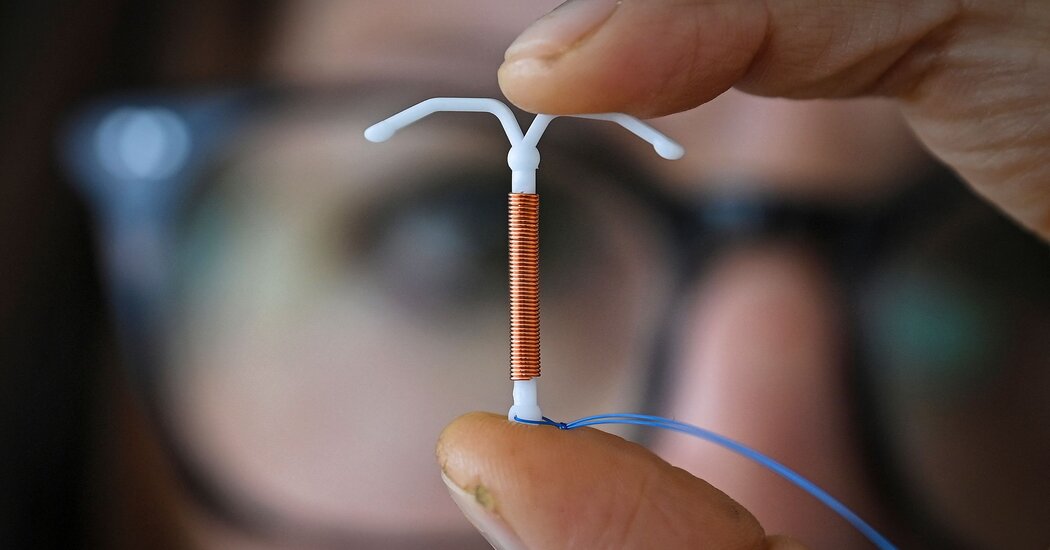
In recent years, the process of getting an intrauterine device, or IUD, has become infamous on social media. Videos of women writhing and crying while the T-shaped contraceptive device is inserted have become macabre online staples.
“Unless you’re living under a rock, you’re aware of the issue,” said Dr. Beverly Gray, an associate professor of obstetrics and gynecology at Duke University.
Doctors have been accused of ignoring the discomfort. For the first time, federal health officials recommended on Tuesday that physicians counsel women about pain management before the procedure.
This updated guidance from the Centers for Disease Control and Prevention may lead clinicians to take the pain more seriously and to consider using anesthetics more often, experts said.
“Women’s pain and women’s experiences have been downplayed throughout medicine,” Dr. Gray said.
“This is really validating that for some people, this can be a really painful experience.”
As the number of women opting for IUDs has risen, so have calls for physicians to address the discomfort associated with the procedure. Some women have described it as “the worst pain imaginable” or likened it to a “hot knife” slowly stabbing them.
Effective strategies for managing that pain exist, though a 2019 survey found that few doctors offered those options. Less than 5 percent of doctors offered an injection of a local anesthetic during the procedure, many instead prescribing over-the-counter painkillers, which have been shown to be less effective.
A study in 2015 found that doctors tended to underestimate the pain their patients experienced during the procedure.
While the last version of the C.D.C.’s guidance mentioned pain management for IUD insertion, Dr. Eve Espey, chair of the obstetrics and gynecology department at the University of New Mexico, said she thought these updated guidelines put a much stronger emphasis on the patient’s preferences and experience.
“I think it is a significant change,” she said. “The guidance on this topic has gone from a more provider-centered focus to a more patient-centered focus.” Anxiety about pain may dissuade women from considering the contraceptive, which is safe and highly effective, she added.
Dr. Antoinette Nguyen, a medical officer in the C.D.C.’s division of reproductive health, said the new guidance emphasized that choices about pain management should be based on “shared decision making,” taking into account patient experiences that may heighten feelings of pain, like anxiety and past trauma.
The new guidelines also broadened the pain-relief options available to women during the procedure, a significant addition since lidocaine shots — the sole anesthetic option mentioned in the 2016 guidance — may themselves be uncomfortable, Dr. Espey said.
The choices now include anesthetic gel, creams and sprays. While Dr. Espey said the evidence showing these topical anesthetics are effective was not “fabulous,” the new recommendations still expand the arsenal of tools that doctors have at their disposal.
“It’s good when the public stamps it’s foot sometimes,” she said.